New blog by Karl Alex Mogaka medical student at Kenyatta University School of Health Science who has completed his elective at the Pari Hospital (Zimbabwe)
A phone call from Dr. Kahiga, the GEMx coordinator changed a rather dull afternoon. I must have been excited to learn that my school had spotted me for an exchange program. Apart from having to travel to a different country, experience a new culture, just having to fly made it more exciting.
Zimbabwe was the destination at the University of Zimbabwe. The exchange was to incorporate clinical pharmacy skills and knowledge for a month-long period. I arrived in Harare well into the afternoon, allowing enough time for Mr. Pozi, our driver to pick us up at the Harare International airport. The city was beautiful in the sky. ‘I will love the stay here,’ I murmured to my colleague Beryl, with whom I would take the elective, as the Ethiopian flight touched down minutes past noon.
Mr. Pozi easily recognized soon us after we checked out and drove as straight to the host institution where Mrs. Rachael, the elective officer, was waiting for us to provide further directions for the elective. Beryl and I spent the rest of the afternoon settling down in the institution. The weeks ahead will be engaging, but we up for it. The dean school of pharmacy, Prof. Tagwireyi was instrumental in drawing a Rota for the four weeks we would spend at his school. We spent the first week at the Drug and Toxicology Information Services (DATIS). At DATIS we were able to gather knowledge on handling of poising cases. Poisoning can be chemical, biological or physical. Most of the cases handled at DATIS were referrals from the rest of the country. It was interesting to get hands-on skills in managing poisoning cases especially ones deemed hard to handle by primary and secondary care facilities.
Mr. Gadaga, the director DATIS was very instrumental in showing us what needs to be done at every step of a referred case. For him, response time and determination of the actual poison were key to helping the patient. He also engaged in running of key tests at the specialized lab that was relevant for the poisoning case at hand. The culmination of this knowledge and skills gathering was a case presentation to the panel of DATIS pre-registration pharmacists.

The weekend was here, and being sabbath keepers, we found a local church for spiritual nourishment. It was home away from home. Mr. Nkobu, a church elder at City Church made sure we came back for the rest of the sabbaths.
Week two was yet another learning voyage. This time we hit the road 345 km west of the capital Harare to a district hospital. Themed as ‘Rural attachment,’ the week-long attachment was aimed at imparting knowledge on health structuring at primary care establishments. We made a visit to a level 3 facility as well as several level 1 facilities. Here, we appreciated the role of a pharmacist at the primary care level. Again, this exposure was very informative since such does not exist in my home country. However, the dominance of alternative medicine at rural establishments did catch my attention. The hospitals admitted that they allowed patients to seek non- conventional interventions for some “difficult cases.”
Week 3 needed some conventional medicine. We regrouped with my colleague. It was evident, the one week apart had us both missing each other. After all, we were the only thing close to home for each other. Prof. Tagwireyi organized for us to join the ward rounds at the Pari Hospital. A rotation at the hematology unit was quite a piece. We got to learn much about blood cancers. It was very fulfilling to suggest some of the management protocols for blood cancers. This case of stage 3 Hodgkin’s lymphoma complicated with anemia had the clinician, Dr. Banaman, seek the input of a pharmacist oncologist.

We also joined pediatric rounds. Here prof. Natoo was quite a bill. Her mastery of the pediatric protocols was just admirable. I loved her involvement with the caregivers of the children in the management plan of the cases.
Gynecology was another stop. We also rotated for four days as the other two. Much of the cases we came across mirrored what we had already encountered at home. However, it was interesting to note the differential management protocols for some of those conditions. The consulting gynecologist was quite patient with us for not knowing the given concepts. But again, we were open to learning as well. We wrapped it up with a rotation at opportunistic infection (OI) clinic which also doubled up as a research center for HIV/AIDS regimens for the Zimbabwe populace. I agree it was much informative.

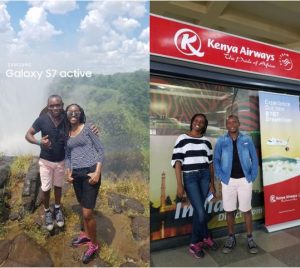
We would not have done justice to the stay in Zimbabwe had we not visited the iconic Victoria Falls. Three days before our travel back home, we made a maiden journey to Victoria Falls, 600km west of the capital. The site of the falls is just breathtaking. We were both in awe all the while as we let the site take our breaths away. The excursion was iced up with a zip-lining experience. The learning experience at the Pari Hospital might have been fatiguing, but this experience was a deserved nerve-calmer. Soon, a flight would touch down at Nairobi JKIA. “Home at last,” I sighed as I checked out of immigrations. The new friends including one Mr. Van would be ones to keep in touch all through.